Since I tend to be a one trick pony and like to tie my blog topics back to my current interests, I’m going to write about Helicobacter pylori, the bacterial species that I am studying. H. pylori is fascinating to me because it’s a big intellectual puzzle; we haven’t determined specifically how it’s transmitted between humans, whether it’s an important gut microbe to be colonized with, and how it specifically causes gastric cancer. However, one of the reasons that H. pylori particularly interests me as a scientist is that it illustrates the difficulties inherent in developing scientific and policy solutions to complicated health problems.
Helicobacter pylori is a bacterium that lives in the stomach of around 50% of people worldwide. It co-evolved with humans for at least 58,000 years and, when present, is typically the dominant bacteria in the gut. In 1984, after observing this bacterium in stomach samples from patients with gastric inflammation, Barry Marshall (one of the scientists who discovered H. pylori 2 years earlier) drank a Petri dish full of the bacteria. He quickly developed symptoms of gastric inflammation, demonstrating that H. pylori can cause gastric distress and that he was willing to go to great lengths to prove it. Since then, H. pylori has been heavily studied, and has been categorized as a class one carcinogen. However, in recent years, there has been a growing body of evidence suggesting that H. pylori may have some positive effects as well.
 The Good
The Good
H. pylori is typically less common in so-called developed nations (the ones with the most money and best public health services). In the US, the number of people who are infected with H. pylori has declined substantially since the advent of antibiotics and extensive protection of the drinking water supply. So has the prevalence of stomach cancer and peptic ulcer. However, there has simultaneously been a substantial increase in rates of esophageal cancer, asthma, allergies, and certain skin diseases. Multiple studies have found a strong inverse association between low asthma rates and infection with H. pylori that produce compounds associated with gastric inflammation. H. pylori expert Martin Blaser and others have suggested that being colonized with H. pylori protects the host against these conditions, but the mechanisms of this are not well understood.
The Bad
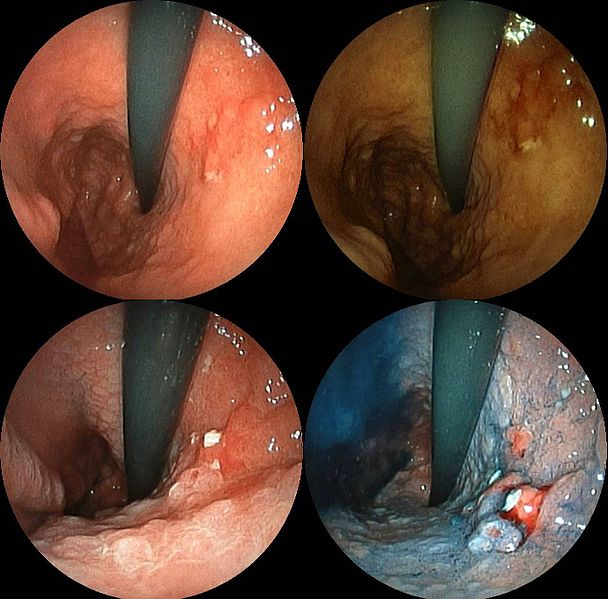
H. pylori is thought to cause much of the world’s burden of peptic ulcers and gastric cancer. Generally, 10% of people who are infected develop peptic ulcers and gastritis, which over time can lead to gastric cancer. Gastric cancer kills an estimated 740,000 people worldwide annually and disables many more, a devastating human cost that also results in billions of dollars of lost productivity. There are many studies that have identified certain compounds that H. pylori produces that are risk factors for peptic ulcer and gastric cancer. However, not all strains of H. pylori that cause ulcers and cancer produce these proteins. Interestingly, H. pylori doesn’t cause symptoms in most of the people it infects, so many people carry it without any negative side effects.
?!?@?#?!?#$?
So, what is the proper way to deal with a tricky situation like this? As a society, we don’t have any set guidelines for dealing with a variable threat/protector like this. In the past, scientists have performed antibiotic therapy for everyone with H. pylori in places with high risk of gastric cancer, even if they did not show symptoms. As resistance to the current antibiotic treatment has increased in H. pylori populations, this may soon not be a viable option in all places; otherwise, we could be producing super-resistant H. pylori, and that’d be a big mess to clean up!
Clearly, more research is needed to determine why some people who are colonized with H. pylori develop disease and others do not. Are there any genetic risk factors in humans that are associated with H. pylori related gastric cancer? Are there any other ways of determining whether strains of H. pylori are harmful? Are there faster ways of determining whether one is infected with a harmful type of H. pylori? All these questions can be chipped away at with proper research, and would help enable physicians to decide more prudently between treatment options. Several studies suggest that eating certain foods may lower the risk and/or mitigate some of the effects of H. pylori infection. The development of a vaccine that would help prevent infection with H. pylori is in the works, but is a long way from being usable.
While far from being implemented (or even accepted in the scientific community), another proposed method of action is selective inoculation, which is similar to vaccination. This would entail infecting people with known benign strains of H. pylori early in life, allowing individuals to reap the protective effects of the bacterium. Selective inoculation would then be followed by antibiotic eradication later in life. However, it seems unlikely that the public would go along with the idea of selective inoculation. If people aren’t willing to give their children an extremely low-risk vaccine, the idea of giving people a potentially cancer causing bacterium could cause some good old fashioned mobbery.
One of the most expensive steps, but also the most helpful, would be reducing the societal factors that contribute to H. pylori infection. One of the Millennium Goals is to reduce the number of households with unimproved water supplies and the provide equitable access to nutrition and health services. Unclean houses, poor nutrition, and lack of access to clean water and sanitation are all strongly associated with H. pylori infection. In and ideal world, this would be a great option, but as there is a lack of funding (especially in lower socioeconomic status countries where it is most needed), figuring out locally implementable ways to handle this could be a good option.
In conclusion, logical policy options to address this problem are not easy to determine, and therefore the most prudent solutions require careful scientific research. The economic costs due to peptic ulcer and gastritis in the United States alone are estimated to be several billions of dollars in lost productivity and hundreds of millions of dollars in medical treatment. Barring a grand global outreach program that would help build high quality water treatment plants and provide clean food and water to the world’s inhabitants, careful scientific experimentation seems like the most promising way to determine the best options for dealing with this challenging bacterium.
Adapted from on Mind the Science Gap http://www.mindthesciencegap.org/2013/11/28/bacterium-many-hats/References:
- Cover, Timothy L., and Martin J. Blaser. “Helicobacter pylori in Health and Disease.” Gastroenterology 136.6 (2009): 1863-1873. DOI
- Linz B, Balloux F, Moodley Y, Manica A, Liu H, Roumagnac P, Falush D, Stamer C, Prugnolle F, van der Merwe SW, Yamaoka Y, Graham DY, Perez-Trallero E, Wadstrom T, Suerbaum S, Achtman M. “An African origin for the intimate association between humans and Helicobacter pylori.” Nature.2007;445:915–918. DOI
- Fischbach, Lori A., et al. “The Association Between Barrett’s Esophagus and Helicobacter pylori Infection: A Meta‐Analysis.” Helicobacter 17.3 (2012): 163-175. DOI
- Amedei, Amedeo, et al. “The effect of Helicobacter pylori on asthma and allergy.” Journal of asthma and allergy 3 (2010): 139-147. DOI
- Wong, Benjamin Chun-Yu, et al. “Helicobacter pylori eradication to prevent gastric cancer in a high-risk region of China.” JAMA: the journal of the American Medical Association 291.2 (2004): 187-194. link
- De Francesco, Vincenzo, et al. “Worldwide H. pylori Antibiotic Resistance: a Systematic.” J Gastrointestin Liver Dis 19.4 (2010): 409-414. link
- Brown, Linda Morris. “Helicobacter pylori: epidemiology and routes of transmission.” Epidemiologic Reviews 22.2 (2000): 283. link
- Zhang, Hong-xin, et al. “Immunogenicity of oral vaccination with< i> Lactococcus lactis</i> derived vaccine candidate antigen (UreB) of< i> Helicobacter pylori</i> fused with the human interleukin 2 as adjuvant.”Molecular and cellular probes (2013). DOI
- Willyard, Cassandra. “A tough controversy to stomach.” Nature medicine15.8 (2009): 836-839. DOI
- Ma, Jun-Ling, et al. “Fifteen-year effects of Helicobacter pylori, garlic, and vitamin treatments on gastric cancer incidence and mortality.” Journal of the National Cancer Institute 104.6 (2012): 488-492. DOI